Introduction
In this feature, we’ll give you an overview of PTSD (Post Traumatic Stress Disorder) with real testimonials and concise, easy-to-read information and advice about treatment options. Whether you are suffering with PTSD, know somebody who is, or just looking to learn, we sincerely hope it helps.
This account, from PTSD sufferer P.K Philips, was posted to the Anxiety and Depression Association of America’s (ADAA) website in 2018.
“For months after the attack, I couldn’t close my eyes without envisioning the face of my attacker. I suffered horrific flashbacks and nightmares. For four years after the attack I was unable to sleep alone in my house. I obsessively checked windows, doors, and locks. By age 17, I’d suffered my first panic attack. Soon I became unable to leave my apartment for weeks at a time”
Although specific cases of PTSD can be as unique as the people who experience them, at least some of P.K’s story will be familiar to people with experience of PTSD.
1. What is PTSD?
“My husband of all of three months had become a shell of his former self overnight. He had gone from a hardworking, compassionate, independent man to someone whose hands tremor so badly he can’t tie his own shoes and has night terrors so vivid he is often hoarse the next morning.”
(Source: Gawker.com)
PTSD stands for Post-Traumatic Stress Disorder. It is an anxiety disorder that occurs in cases where an individual has experienced (or been otherwise exposed to) stressful, frightening or distressing events.
Although it is best known for affecting veterans and military personnel exposed to combat situations, PTSD can actually occur from a varied and diverse array of circumstances, including:
- Road accidents.
- Assault (including sexual assault).
- Burglary/Home invasion.
- Serious health problems.
- Experiences during childbirth.
- Torture.
- Harassment/Bullying/Stalking.
- Being kidnapped/Held
- Hostage.
- Surviving a natural disaster.
- Bereavement.
- Imprisonment.
- Any event in which a person fears for their life.
In simple terms, PTSD occurs when a person’s mind is unable to integrate unwanted memories in the usual way.
These memories (which can include emotional reactions and sensory experiences) can then intrude upon that person’s life in a variety of different ways, including flashbacks, nightmares, emotional outbursts and physical symptoms such as shaking or panic attacks.
The condition is far more common than most people realise, as it develops in about 1 in 3 people who experience severe trauma.
2. History of PTSD
“He gave a clear description of nightmares, vivid dreams, visual flashbacks, and he can also smell burnt flesh and feel the smell of death… He also described (…) tensing up when he saw hazard-warning lights on a vehicle. He explained that in Iraq, vehicles loaded with explosive devices only had their hazard warning lights on.”
(Source: The Guardian)
PTSD has probably been around for almost as long as human beings have. Examples of what would now be viewed as PTSD occur throughout our historical records, though the chroniclers of their time often lack the terms to properly describe it.
In 480BC, for example, Spartan commander Leonidas is recorded as dismissing men from the battlefield if they were too psychologically affected by previous battles. In another instance from antiquity, the Greek Herodotus describes an Athenian soldier who went blind from fear during the battle of Marathon.
In 1678, Swiss military doctors recognised the symptoms of PTSD, then grouped them together under the term ‘nostalgia’. Later, troops fighting in the American Civil War were diagnosed with ‘soldier’s heart’ or ‘exhaustion’.
During the First World War, the condition was identified as ‘shell shock’ because it was believed that the explosions of bombs and shells caused nerve damage. By the conclusion of the Second World War, where more than 43% of all men discharged were sent home with psychological trauma, the terminology had been softened to ‘battle fatigue’.
 In the 1950’s, as a better standard of medical science began to emerge, the condition became known as ‘stress response syndrome’.
In the 1950’s, as a better standard of medical science began to emerge, the condition became known as ‘stress response syndrome’.
Following the Vietnam War, as more and more veterans were diagnosed with ‘post-Vietnam syndrome’, there was intense pressure for both the medical community and military organisations to better categorise and treat this elusive ailment.
Since that time, PTSD is understood to impact the lives of a great many people, even if those people are not soldiers. In fact, female victims of rape develop PTSD in far greater numbers than male war veterans do.
Compare these excerpts to the testimonials shared throughout this article and you’ll see that PTSD has a long and sad history.
3. What Causes PTSD?
“Until you kill other human beings for survival, what could you possibly say about it? It assaults all your scenes, the smell of death and the machines that cause it. Noises so loud you feel like an ant under a lawnmower. It is incomprehensible”.
(Source: Gawker.com)
We now know that trauma, of any kind, changes both the brain and the body. Every trauma-related neuropathway, even if it has lain dormant for a considerable period of time, has the potential to reactivate.
In the ‘Triune‘ (or ‘three part’) brain model, the brain is separated into three parts, the reptilian (responsible for instinctive and autonomic behaviour), mammalian (which processes emotions and senses) and neomammalian (which controls cognitive learning, decision-making, learning and memory).
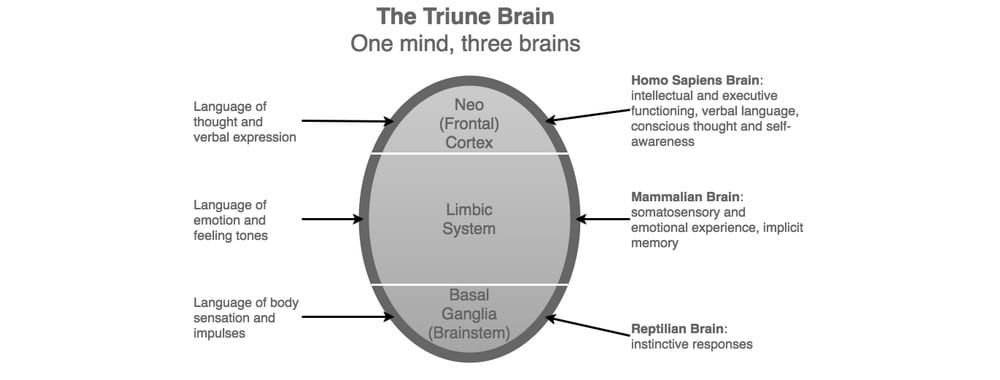 During a traumatic event, the reptilian brain takes over, mainly to facilitate a quick escape. You often hear survivors of natural disasters or terrorist attacks saying things like “I didn’t think, I just acted” this is because the reptilian brain forcibly shuts down all non-essential body and mind processes. The sympathetic nervous system then releases all the ‘fight or flight’ hormones necessary to survive. This is called ‘reactive mode’.
During a traumatic event, the reptilian brain takes over, mainly to facilitate a quick escape. You often hear survivors of natural disasters or terrorist attacks saying things like “I didn’t think, I just acted” this is because the reptilian brain forcibly shuts down all non-essential body and mind processes. The sympathetic nervous system then releases all the ‘fight or flight’ hormones necessary to survive. This is called ‘reactive mode’.
Once the person has survived, the parasympathetic nervous system begins to reassert control, reducing the stress hormones now that the threat has passed. This is called ‘responsive mode’.
In some cases where PTSD develops, the transition from reactive to responsive mode never actually occurs. Instead, the reptilian brain maintains its grip on the individual, giving them a constant feeling of being under threat.
Imagine that your brain never stopped feeling like it did when that car almost hit you, or when that gang of big kids cornered you in childhood, or when somebody you loved was about to die and you were powerless to help them. Now imagine those feelings lasting years, even decades. That, in effect, is PTSD.
4. Symptoms of PTSD
“Even after I moved to Germany, removing myself from the city and the country where the burglary occurred, the robbery stayed with me. It took weeks before I stopped having bad dreams or stopped eyeing strangers on the street near my house. The most valuable thing the burglars took was my sense of security”.
(Source: Pacific Standard)
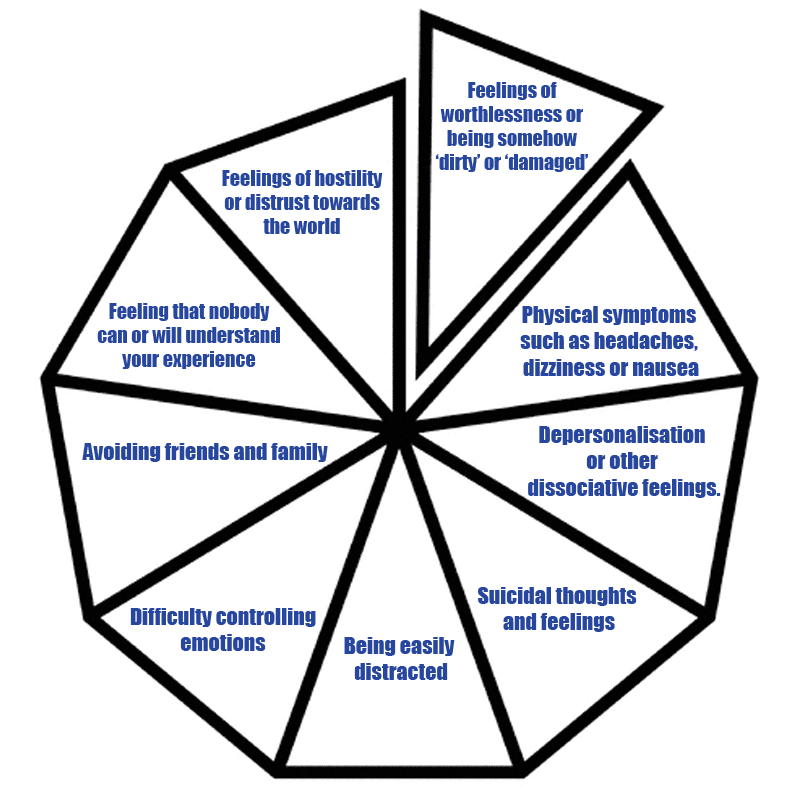
Generally speaking, PTSD symptoms fall into four main groups. These are:
- Intrusive thoughts (unwanted memories or flashbacks).
- Mood alterations (becoming excessively negative or irritable).
- Hypervigilance (being constantly ‘on edge’ and having an exaggerated startle response).
- Avoidance (going to great lengths to avoid anything that reminds the sufferer of the traumatic events).
PTSD may present via nightmares, flashbacks, mood swings, violent fits of rage, increased heart rate, pain, chest pains, panic/anxiety attacks, sweating, nausea, shaking, memory loss, forgetfulness, insomnia, shortness of breath, crying, emotional numbness, isolating oneself from friends, family and colleagues, low self-esteem, self-harm, self-destructive behaviour and abuse of alcohol or drugs.
Some PTSD sufferers experience complex feelings of guilt or shame relating to their experiences. They can exhibit trust issues or feelings that nobody understands them. Some feel that they can never be safe. They may become suspicious, even paranoid. In some cases, PTSD sufferers have become completely unable to express affection for other people.
In children, PTSD can present through bedwetting (or other ‘accidents’), anxiety about being separated from a parent or trusted adult or re-enactment of the trauma through play.
5. How to Tell if you Have PTSD
“The depression totally immobilises me. I can’t even pick up a razor to shave, unable to look in the mirror; I question my existence. It becomes so intense that I have to go to bed for a couple of days and wait for it to pass.”
(Source: NCBI)
If you’ve experienced a traumatic event at any point (even during childhood), you may develop PTSD as a result. If you are experiencing any of the symptoms described above on any kind of a regular basis, you may already have PTSD.
Fortunately, there are a number of tests available online. Click the link below and see for yourself.
 If you have doubts, you should consult your doctor.
If you have doubts, you should consult your doctor.
A good idea would be to talk to a trusted friend, family member or partner. Ask them if you seem different or if your behaviour has changed.
Think back to a time before the traumatic event took place. Did you do anything differently? How has the event changed you?
The answers may surprise you.
6. PTSD Diagnosis
“Triggers can come from anywhere at any time… a smell, a look/ glance, a vibe, a dream… how someone treats you. You are unable, as hard as you try, to turn it off.”
(Source: The Mighty)
After a traumatic event has taken place, it is normal to experience feelings of anxiety, sadness or stress. Sometimes the event will play on your mind or stop you from sleeping, but these effects should only be temporary.
It is also normal for some people who don’t have PTSD to exhibit some of the symptoms of PTSD. This does not necessarily mean that they have the disorder.
It is very common these days for people to look up their symptoms online and immediately assume the worst (headache = brain tumour) and this is as true for mental ailments as it is for physical ones. Many PTSD symptoms are also symptoms of stress, for example.
The criteria for diagnosing PTSD consists of 8 points, labelled A – H. Patients must fulfil said criteria in order to be formally diagnosed.
However, only a medical professional can do this. If you are concerned about yourself or somebody else, we recommend taking one of the quizzes we’ve linked in this piece and following that up with a visit to your doctor.
7. What Does a PTSD Diagnosis Mean?
“I was diagnosed by my GP with PTSD a few weeks after the death of my father who died very suddenly, following a family outing to the local pub for lunch. He collapsed in front of us and we had to administer CPR at the scene while waiting for the ambulance. He died on his way to hospital.”
(Source: Mind.org)
If you have an unpleasant or frightening experience, it is normal for your emotional reaction (e.g. fear, panic, anger etc.) to outlast the event itself. Usually, these feelings will fade over time. However, if they do not, you could be experiencing PTSD.
Being diagnosed with PTSD (or any other psychiatric disorder, for that matter) does not make you ‘crazy’ – nor is it a sign of weakness.
PTSD does not describe cowardice or even an ‘inability’ to deal with unpleasant events. It is the natural consequence of a human mind that is trying to process a traumatic experience.
Additionally, you don’t have to directly experience trauma in order to develop PTSD. If a person close to you experiences trauma of any kind, it is possible for you to develop PTSD from this. In some instances, police officers have developed PTSD after repeated exposure to the unpleasant details of child abuse or murder cases, even though they were never physically present for any of the events described. This is called secondary trauma.
8. What Does PTSD Feel Like?
“I was still mentally and nervously organized for War. Shells used to come bursting on my bed at midnight, even though Nancy shared it with me; strangers in the daytime would assume the faces of friends who had been killed.”
From an account given by Robert Graves, British poet and veteran of the First World War (Source: Washington Post)
Living with PTSD can be a constant challenge. Some sufferers have described it as being similar to the feeling of anxiety or alertness after someone or something suddenly scares you, except that it never goes away. Others describe a feeling of being constantly on guard.
According to some descriptions, it is a feeling of being perpetually trapped in a terrible moment of time, for others, it is, quite literally, a waking nightmare.
A PTSD sufferer named ‘Nargis’ gave a particularly evocative description of the disorder to the health website ‘The Mighty’
“It’s like you’re tidying your house before a dinner party. But there’s this one item that’s just out of place. The doorbell rings. It’s your guests. You just shove that item into the closet and tell yourself you’ll deal with it later.
You start to do this every time. Filling the closest more and more. Saying to yourself that you’ll deal with it later. The closet becomes so full that it starts to creak.
That’s your bodies way of saying ‘Hey! You got a lot of stuff to deal with! It’s time!’ But you keep thinking it’s fine.
Out of sight, out of mind. You ignore the closet. Until one day it’s too much. The closet bursts. And everything comes flying out in weird and wacky ways. Panic attacks. Dissociative episodes. Depression. Anxiety. Flashbacks. Intrusive thoughts.
And then you’re left lying on the floor with all the items that were stuffed into the closet, splattered around you. Forced to finally accept what happened. And forced to finally deal with it.
Forced to clean up the items around you and find appropriate places for each thing. And then over time, slowly, you learn what to do with each item, and how to deal with each thing, uniquely.”
9. How Long Does PTSD Last?
“I found my therapist very easy to talk to, understanding, a good listener and very helpful. The treatment he provided definitely helped me get over this traumatic time in my life”.
(Source: NCBI)
There is no set duration for PTSD, but the good news is that it rarely lasts forever. In some extreme cases, it can bother a person for the duration of their life, but modern therapy has a high success rate and can at least lessen PTSD symptoms in such cases.
Very often, PTSD can be completely overcome. It takes time and hard work, but the condition is actually very treatable.
Symptoms are unlikely to go away by themselves, however. Treatment of some kind is most likely essential (more on this later).
Factors that influence the duration of PTSD include the amount of times the trauma was experienced, whether it was accidental or intentional, whether or not the initial trauma was sexual in nature, prior experience of other mental conditions such as anxiety or depression, the level of social support a person has and their willingness to engage others for said support.
As stated earlier, each case is different, so there is no viable timetable.
10. Treatment Options for PTSD
“The thing that has been most helpful on this journey has been counselling. Friends and family can’t always understand what and why I feel the way I do, but counsellors are always there to listen. I have been in therapy almost a year now, yet I do believe that you need to find a counsellor you can click with. I tried a couple before I found the right one, but just knowing you can share with someone, who is not going to judge you and be there for you through dark times, has really helped me”.
(Source: Time-To-Change.org)
PTSD can be treated, and even defeated. Most cases of PTSD are not lifelong and, even in cases where the condition persists, therapy can greatly reduce the symptoms.
Therapists pursue three main goals when treating a PTSD patient. The first is to improve the symptoms, the second is to teach the patient some skills that can deal with the symptoms and the third is to restore the individual’s self-esteem.
The most common (and effective) treatment technique used by PTSD sufferers is Cognitive Behavioural Therapy (CBT). CBT teaches methods by which the patient can ‘take back their mind’ as it were. Often, negative thought patterns continue unchallenged in the sufferer’s mind, even as she or he yearns desperately for peace. CBT teaches the patient to break these patterns, using techniques that have a very high success rate with PTSD patients.
Stress Inoculation Training (SIT) is part of CBT, and teaches a number of stress reduction techniques (such as breathing to stimulate the vagus nerve). These are tried and tested techniques that are proven to reduce anxiety.
Other forms of treatment available include support groups (especially successful if the PTSD stems from an event that affected a lot of people besides the patient, e.g. an industrial accident, a war or a natural disaster).
Some group therapy (for example groups pertaining to sexual assault, incest or domestic violence) can also be very useful, as it helps patients to talk with people that have experienced the same thing. Sometimes, simply understanding that their feelings aren’t unique to their ‘crazy’ brain and are in fact a normal human response to a perceived threat can be a huge step on the road to recovery.
Cognitive Processing Therapy (CPT) is a 12-week program consisting of weekly 60 – 90 minute sessions. During these sessions, the patient is asked to talk through the traumatic event in detail and also to write their experiences down. This helps a therapist to highlight unhelpful ideas and thought patterns that are impeding the patient’s recovery.
Prolonged Exposure Therapy (PET) helps the patient to confront the event(s) and their feelings about it/them. This is mostly used in cases of avoidance. Patients are recorded describing their trauma and then listen to the recordings at home, this helps them face up to the past and put it behind them.
If you really don’t feel that you can talk about what happened (a lot of people can’t – this is a common PTSD symptom), you can receive Eye Movement Desensitization and Reprogramming (EMDR) treatment. For this therapy, the patient is asked to think about their trauma while a therapist encourages them to replace negative thoughts and attitudes with positive ones. It usually takes about three months to be effective.
In some cases, medication may be prescribed. Drugs that affect neurotransmitters like serotonin and norepinephrine (SSRIs & SNRIs) can help to ‘re-balance’ the way the patient’s brain processes fear and anxiety. Other drugs, such as beta-blockers, antidepressants and benzodiazepines can work for a limited time to ‘soften’ a patient’s PTSD experience.
Many of the anxiety reducing techniques mentioned here are available online, so even if you feel that you cannot face a therapist right now, you can work on reducing your anxiety this way until you can.
Remember also that therapy is confidential – and that there’s nothing you can tell a professional therapist that they haven’t heard before.
Whatever you do, don’t feel that you can’t go through with therapy, or that you’re a ‘lost cause’ if one particular technique doesn’t yield results. You are much stronger than you think you are.
11. Coping With PTSD
“I now understand why I behave the way I do. I believe it was a very important part of my recovery, as I have been given the tools to help myself and put them to use as soon as I could. I have learnt to recognise certain feelings, which I’ve discovered are triggers, and stop any negative behaviour”.
(Source: NCBI).
Often, PTSD arrives in the form of ‘habits’. Because the patient thinks about the event so often, they have a habitual way of relating to it and experiencing thoughts about it. Avoidance, too, can become habitual, as can low self-esteem, self-destructive behaviour and many other PTSD symptoms. Over time, PTSD becomes a part of you, but it doesn’t have to stay that way.
Imagine a person that is in the habit of eating junk food at all times of the day or night, they will gain weight and suffer the associated health problems from this habit. However, if they can instead change their habits to mainly eating healthy food and at set times in the day, they will lose weight and suffer less as a result. Your mind works in basically the same way. The traumatic event is in the past; it now exists only as a memory. Change the habitual way you think about the event – and you can change what the memory means to you.
If you are experiencing regular flashbacks, it helps to learn some breathing exercises. It also helps to carry an object that reminds you of the present. Use it to remind yourself that you are somewhere else now, not still experiencing past trauma. Assure yourself that you are safe and (if you can) take comfort in something that soothes you. Try also to focus on your surroundings, or even describe them out loud. Stay safe in the moment and try not to let your mind drift from the present. It may also help to keep a diary because this will help you to identify your triggers.
Knowing your triggers is very important. A trigger is something that brings about your PTSD symptoms (often in the form of flashbacks). It could be anything, from an anniversary that reminds you of the event, to a smell, or even a song on the radio.
Once you identify these triggers, you have taken a major step forward. Not only can these triggers be better avoided once you understand them, but it will also now be easier for a therapist to understand and help treat your symptoms.
Developing a routine for sleep and preparing your mind and body for bed each night can also help. Sleep is enormously beneficial to the body and mind. This will be difficult at first, but keep in mind that all things are possible with practice.
It will also help if you can confide in someone. This could be a therapist or a support group, but these things work particularly well when balanced against the support of a trusted friend, partner or family member.
You might also consider the practice of gratitude. Gratitude, as they say, is a habit that becomes a way of life. To start off, simply spend 5 – 15 minutes each day mentally or verbally listing things you are grateful for/happy about.
Do not focus on fears, anxieties or things you find upsetting during this time, only the good. It could be things as basic as “I’m grateful for the food in my belly, the roof over my head, the air in my lungs and the love in my heart”. You can express gratitude for your family, your friends, or even a show you’re enjoying on TV.
Eventually, this process internalises and sees you focussing more on what works in your life than what doesn’t. It doesn’t matter what or whom you are expressing gratitude to.
You needn’t add any kind of religious or spiritual element, simply be grateful and happy to be alive. It sounds a bit mad, but trust us – it works. Meditation can also be greatly beneficial.
Avoid abusing alcohol and/or drugs. These things may feel as if they help, but they really don’t, especially over the long term. As a PTSD sufferer, you are in a precarious place – and these substances can worsen your situation very quickly.
Try also to improve your diet and, where possible, get more exercise (running can be especially useful). These things affect the body in several key ways – and actually contribute to a person’s happiness and positive mental state in some surprising ways.
Above all, be patient. Developing mental habits deliberately takes both time and effort. You will slip up, you will have bad days – and it is difficult at first, but stick with it. Have faith in yourself and hope for the future and you’ll rarely be disappointed.
12. How to Support Someone who has PTSD
“Being the partner of someone who has PTSD can be challenging — and frustrating — for many reasons. You want to take away their pain, but you’re also dealing with your own guilt at needing to care for yourself, too”.
(Source: Healthline.com)
PTSD can – and has – torn families, relationships and entire lives apart. Even today, it is still a very misunderstood disorder. Mental health is still a ‘taboo’ subject and is very difficult for most people to talk about.
Caring for someone with PTSD can be very difficult. First of all, keep in mind that it is neither your job, nor your duty to ‘cure’ or ‘fix’ the person. You cannot do this – and if you try, you will likely fail and make the situation worse. Your job is to provide social support and help, nothing more.
Do not pressure the person into talking. If they are reluctant or unwilling, this will likely cause more problems than it solves.
Encourage normalcy in their life. Remind them if they haven’t indulged their hobbies in a while and gently encourage them to socialise with others. It may also help to find regular activities you can do together, such as fitness classes, art classes or regular shopping trips – whatever you both enjoy. If you haven’t the money, try walking or having ‘movie nights’ at home.
Be patient with them. You may have to endure some ‘difficult’ or irritating behaviour – just keep in mind that by not reacting negatively, you’re doing them a favour. Don’t let yourself be pushed around or abused in any way, but equally don’t go on the offensive. Simply remove yourself if the situation becomes too negative, but always keep the lines of communication open when you do. It helps to understand and anticipate their triggers and watch for signs of anger, stress or discomfort.
Listen to them, but don’t give them instructions on how to cope. Everyone is different. Don’t blame all their/your problems on PTSD. The condition may contribute to the problems, but it won’t be the entirety of them.
Don’t turn the conversation around to your own experiences; even if they are the same as the other person’s. Everyone is unique, including the way we relate to and process trauma.
Avoid shaming them or making them feel guilty. Never trivialise or make fun of what they’re going through. Do not, under any circumstances, tell them to “just get on with it”.
Research PTSD. This feature is a good start. To find out more, try clicking the links scattered throughout this piece. You can also find a wealth of information and documentary films like THIS ONE.
Above all, take time for yourself and look after yourself. Your life is just as important as anybody else’s. You may feel duty-bound to care for the person every waking minute, but you will soon burn out if you try to – and you could end up invoking feelings of guilt in the other person if you do.
Keep yourself as fit and rested as possible, remain engaged with your hobbies and interests, take time for yourself. Keep empathy and compassion at the core of everything you do.
More advice, if needed, can be found HERE
13. PTSD in Popular Culture
“He is in a constant state of stage fright, he says, because he never knows what part of his life he is going to have to act in next.”
Excerpt from ‘Slaughterhouse-Five’, by Kurt Vonnegut, (Source: Thought Co)
In the case of PTSD, it took a relatively long time for psychologists to catch up with popular culture, which had been exploring the disorder for centuries.
The American Psychiatric Association (APA) did not add PTSD to its ‘Diagnostic and Statistical Manual of Mental Disorders’ until 1980, yet children in the US had known about PTSD since at least 1939’s ‘Detective Comics’ Issue 33, whereupon Batman’s violent origin was revealed to young readers.
Since then, Bruce Wayne’s flashbacks, avoidance of certain objects (guns) and recurring nightmares (all textbook PTSD symptoms which stem from the violent deaths of his parents) have been shown almost constantly, making the Batman comic books arguably the longest continuous exploration of PTSD in the entirety of English literature.
In fact, the list of fictional characters that experience some form of PTSD is long and varied. Here are a few more examples:
- Tony Stark in Iron Man 3, suffering from PTSD after fighting Loki and Thanoses’ army
- Will Hunting in ‘Good Will Hunting’ (PTSD from an abusive childhood).
- Jenny Curran in ‘Forest Gump’ (PTSD resulting from child sexual abuse). Also Lt. Dan Taylor in the same film (combat experiences).
- Harry in ‘Harry Potter’ (PTSD from neglectful/abusive childhood, violent death of parents).
- Jeff Bauman in ‘Stronger’ coping with the 2013 Boston Marathon bombing.
- Captain Picard in ‘Star Trek: The Next Generation’ (suffers from PTSD after being assimilated by The Borg, this is especially true in the film ‘First Contact’).
- Both Willard and Kurtz in ‘Apocalypse Now’ (PTSD from issues relating to combat experience).
In general, books, film and television tend to use PTSD symptoms as a quick way of adding depth to a character. However, the long-term struggle that PTSD represents usually takes place away from the main narrative.
Lazy writing and armchair psychology also play a large part in misrepresenting this disorder (and many others) to the public at large.
On the one hand, the amount of PTSD seen in mainstream media can be good for creating awareness, on the other hand, the many inaccuracies and ‘quick fix’ resolutions can also be counter-productive. Often, PTSD is reduced to a simple storytelling trope – and rarely is it even mentioned by name.
Nevertheless, there are a growing number of accurate, sensitive and thoroughly researched portrayals of PTSD in books, video games and on stage and screen.
14. Who Can Develop PTSD?
“It is well known by now that prisoners have a much higher prevalence of post-traumatic stress disorder than the general population, ranging from 4% to 21% of the sample. Many more females than males are affected by PTSD in prison”.
(Source: News-Medical.net)
Anybody can experience post-traumatic stress disorder, although women are statistically more likely to develop symptoms, especially in instances when sexual violence is perpetrated against them. Some figures suggest that 50% of all female rape victims develop PTSD as a result.
On average, women are exposed to more ‘high impact’ trauma from a younger age than men, which explains why women experience more PTSD.
According to the latest research, men are most likely to develop PTSD symptoms between the ages of 41 and 45, whereas women are more likely to do so between 51 and 55.
Common causes of PTSD include car accidents, assaults, muggings, home invasion, seeing others being hurt or killed or a painful bereavement.
You are at a greater risk of developing PTSD if you,
- Experience the trauma repeatedly instead of just once.
- Are physically hurt as a result of the trauma.
- Push family, friends and therapists away, isolating yourself.
- Are dealing with extra stress at the time the trauma occurs (e.g. money worries, a break-up or a bereavement).
- Have previously suffered with anxiety or depression.
15. What is Complex PTSD?
“Particularly abusive parents deepen the abandonment trauma by linking corporal punishment with contempt. Slaveholders and prison guards typically use contempt and scorn to destroy their victims’ self-esteem. Slaves, prisoners, and children, who are made to feel worthless and powerless devolve into learned helplessness and can be controlled with far less energy and attention. Cult leaders also use contempt to shrink their followers into absolute submission after luring them in with brief phases of fake unconditional love.”
Excerpt from the book ‘Complex PTSD: From Surviving to Thinking’ by Pete Walker.
Complex PTSD (sometimes abbreviated to CPTSD) usually occurs when a person has repeatedly experienced traumatic events over an extended period of time. This is especially the case if the trauma occurred during the person’s childhood. However CPTSD is not limited to instances of childhood trauma.
In cases of child abuse, neglect or abandonment, CPTSD can be worse if a parent or carer inflicted the trauma upon the child and if that child was otherwise alone when the trauma occurred. It can be especially damaging if the person is still in contact with those responsible for the trauma.
CPTSD manifests in much the same way as ‘standard’ PTSD (if such a thing exists), but can be more difficult to manage and treat due to the repeated nature of the trauma that caused it.
Some symptoms of CPTSD include,
Many people with CPTSD suffer from profound trust issues stemming from their negative encounters with other people. This can make them slightly harder for a therapist to treat.
However, even in the most extreme cases, CPTSD can still be treated and the patient’s quality of life can almost always be improved.
16. Where to Get Help
“I was diagnosed with post-traumatic stress disorder earlier this year. I realise now that I’ve been ignoring the symptoms for a long time. I was partly in denial and partly worried about telling people because of their reaction. I refused to tell work what was going on until I ended up in hospital. I was aware of the stigma around mental health at my workplace and kept everything a secret”.
(Source: Time-To-Change.org).
In most cases, PTSD can be treated successfully. The events that caused the disorder to occur have already happened, that cannot be changed. However, their effect can be diminished as those memories become better integrated and understood by the psyche. CBT and other techniques are giving people their lives back every day – and our understanding of PTSD and other, related disorders is increasing rapidly as well.
If you are experiencing more than a few of the symptoms presented in this piece, or detailed elsewhere in the accompanying links, you should consult your doctor as soon as you can.
Your doctor will be qualified to perform an initial assessment before referring you to a specialist. In the UK, you will need to have experienced symptoms for at least 4 weeks before you’ll be eligible to see said specialist (unless symptoms are particularly severe, of course). You may be referred to a community psychiatric nurse, a counsellor, psychologist or a psychiatrist. If you can afford it, private psychiatrists are available throughout the country. In all cases, these people are qualified professionals who have worked on many cases just like yours.
It may take you a while to find a therapist you ‘click’ with, or it may happen right away. The only advice we can give is to be as honest with yourself as you are with your therapist and to be courageous.
Information available here and elsewhere online should only be used as a starting point. Forums and social media groups can be supportive and useful, of course, but they will be very unlikely to provide you with the ability to treat yourself. Sooner or later, you will need to see a therapist.
This free, printable leaflet contains more information. Remember, it is never too late to seek help. You are more supported, loved and respected than you probably think. Never be afraid to let people surprise you.
For more information about PTSD click here: Singlecare.com
Article and most pictures from PTSD: The Definitive Guide. Reprinted with permission.